How to get enough calcium for your bones
Bone is a dynamic material and is constantly being broken down and rebuilt throughout life. In fact, your entire skeleton is replaced every 10-12 years. It is common knowledge that you need calcium rich foods to support your bone health. In a world where we are turning away from one of the best sources of calcium – milk and dairy products – we need to pay attention to this mineral to avoid trouble down the line. The issue discussed in this blog is how to make sure you are getting enough calcium for your bones and how much you need.

What are bones made of and how calcium fits in
Calcium is the most dominant material in your bone structure. It is delivered to a soft criss-cross matrix with the help of Vitamin D and used to fill the gaps and harden the structure. We tend to reach peak bone density at around age 25 years. It makes sense that if you have good bone density at that age, then you stand a better chance of maintaining bone health later in life. This is an important consideration if you have youngsters at home who are turning away from dairy products and towards alternative milks with lower calcium levels.
Bones also act as a store of calcium, which is a mineral needed for other processes such as cell signalling and muscle function. If your dietary calcium intake drops, signals are sent to your bones to release some into the circulation to restore blood levels for use elsewhere. Your bones can cope with this in the short term. However, if dietary levels remain low in the longer term, you could be losing bone density.
What other nutrients – besides calcium – do your bones need?

Besides calcium, our bones need other nutrients too. Vitamin D helps the body absorb calcium from the diet; magnesium is important to slow down bone breakdown; collagen gives bones flexibility, Vitamin C is used in the manufacture of collagen; Vitamin K is involved in the manufacture of osteocalcin, which in turn helps to harden calcium in the bone structure. There are others – manganese, boron, B vitamins, zinc and more. So we do need to eat a varied and interesting diet to support our bone health. Here we focus on calcium for your bones.
Calcium for your bones – the role of your digestion
Good levels of stomach acid are required for optimal absorption of calcium.
Do you:
- struggle to digest protein foods?
- eat smaller meals as your usual portions now leave you feeling overly full for long periods?
- see undigested food in your stool?
- feel bloated after eating?
- feel nauseas when taking supplements?
If you have answered yes to some or all of these questions, then speak to a nutritional therapist. They can be signs that you need to work on your stomach acid levels. Likewise, if you routinely take Omeprazole or other stomach acid suppressing medication, seek help from a qualified nutritional therapist. PPI medication compromises your ability to absorb nutrients from your food. You are welcome to book a free call with me to discuss how changes to your diet may help with this.
Bone Remodelling
From about age 40, the rate of bone formation tends to slow, with a much sharper decline from about age 50, particularly for some women around the time of menopause. A focus on dietary calcium and other bone nutrients is essential to avoid bone density decline and an increased risk of fractures from minimal impact. The most severe consequence of bone density decline is osteoporosis, which literally means ‘porous bone’, when the usually dense matrix of bone becomes filled with tiny holes.
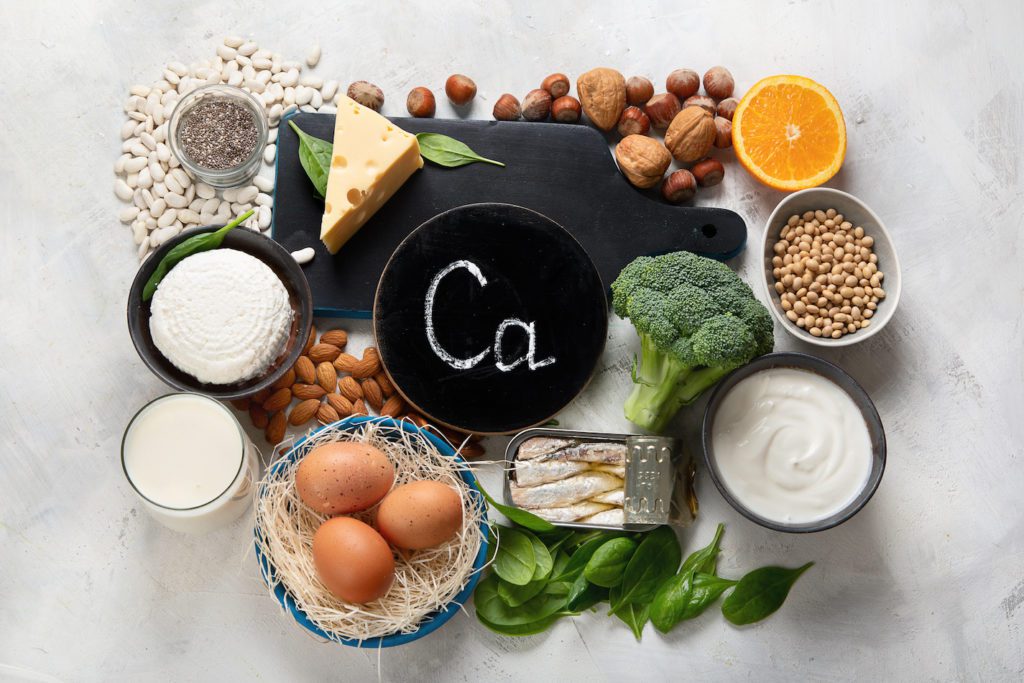
Food sources of calcium for your bones
So, what are the best sources of dietary calcium? Here is a short list, including both dairy and non-dairy foods:
- Whitebait
- Sardines
- Tinned salmon
- Fermented plain live yoghurt
- Cottage cheese
- Leafy green vegetables
- Almonds
- Sesame seeds
- Pulses

The NHS recommend a daily dose of 700mg of calcium from your diet for adults aged 19-64. More is required for children and teenagers and may be needed for those 65 and over. The USA recommendation is higher at 1,200mg daily.
How to make sure you are getting enough calcium for your bones
The table below gives you some suggested daily meals that would achieve your dietary calcium intake:
| Breakfast | Lunch | Dinner | Total calcium |
| Bowl of natural yoghurt with fruit and granola c. 450mg calcium | Mashed sardines and rocket wholemeal sandwich c. 350mg calcium | Mixed poke bowl with black beans and tahini dressing c. 250mg calcium | 1050 mg |
| Banana and almond pancakes with berries c. 250mg calcium | Mixed salad leaves, including 2oz of cheddar cheese c. 400mg calcium | Tofu and broccoli stirfry with rice c. 350mg calcium | 1000 mg |
Calcium content in food varies, so these figures are estimates only. There are traces of calcium in many other foods, so it is possible to achieve good calcium levels in the diet.
Other ideas include:
- 2 oz cheddar cheese (400mg)
- 4 spears broccoli (180mg)
- Large handful spinach (240mg)
- Porridge oats (150mg)
- 2 tbsp tahini (130mg)
- 4oz tofu (varies between 250 – 750mg)
Supplement sources of calcium
If you have worked on your diet and still struggle to get sufficient calcium then you can look to supplementation. You will also need to consider supplementation if you have been given a diagnosis of osteoporosis or its precursor, osteopenia.
Calcium Carbonate
If you have a diagnosis of osteoporosis, then it is very likely that you will be prescribed a medication to support your calcium and Vitamin D levels, such as AdCal D3. This contains calcium in the form of carbonate, which is basically a chalk. Each tablet contains 1500mg of calcium carbonate, which translates into 600mg of elemental calcium. The standard dose is 2 tablets daily. You need this high dose of calcium in this form because it is poorly absorbed.
Other types of calcium
Food sources of calcium are always best, but when supplementation is necessary, I prefer to use calcium in the citrate form. This is much better absorbed and therefore it is possible to take a lower dose than the carbonate form. Dosing recommendations are made dependent on bone health and dietary intake. I work in collaboration with my clients’ GPs when making these changes in the best and safe interests of my clients.
The importance of not getting too much
When there is too much calcium through diet and supplementation, then it can cause a situation of hypercalcaemia. The knock on effects of this can be as mild as constipation, to as serious as kidney stones, heart function problems and confusion. So it is important to work with a qualified nutritional therapist together with your GP to get your calcium levels optimal – not too low, not too high, just right.
If you have been diagnosed with osteoporosis and would like to discuss your own situation and how nutrition and lifestyle changes may be able to help, you can book a free call with me. I’ve worked successfully with clients, who’s follow-up DEXA scans show improved bone density. It is worth investing in your health so you can get your life back on track. Call me to find out more.
If you are looking for some recipes, grab a free eBook with 10 delicious recipes focusing on cruciferous vegetables. Good for our livers and the creation of the master antioxidant, glutathione, which can help modify pain. Grab it here!
